About this app
This technology aims to engage people who:
- are interested in healthy ageing
- may have a health or other predisposition to dementia
- are noticing early changes in their cognitive health.
The app helps users:
- identify modifiable risk factors that may increase their chance of developing dementia later in life
- start a conversation with their GP about brain health and risk-reduction strategies
- set brain-healthy goals to reduce risk and optimise their brain health
- monitor their cognitive performance over time
- recognise cognitive change and promptly seek help
- access reliable information, advice and strategies.
This app does not replace a formal cognitive assessment.
How often do you use the app?
The app is a self-monitoring tool designed around a travel narrative. Users travel to a new country every 30 days to complete a series of games. Each game is adapted from validated cognitive testing and targets a specific cognitive domain.
How to optimise your results
To get the most out of this app:
- choose your best time of day to concentrate
- make sure you can see the screen
- make sure your sound is on
- choose a quiet space where you won’t be interrupted.
Do not worry if you make a mistake. Your results are measured over time. Results are a starting point for conversations about brain health.
Further information about what to do with your results.
What do the games test
Each game within the app focuses on specific cognitive domains. Unlike validated cognitive screening tools, this app is not designed to be diagnosis-specific or diagnosis-sensitive. It simply highlights concerns in specific areas of cognition.
Many atypical cognitive conditions are not detected through standard cognitive screening tests. For example, a person with cognitive changes affecting their frontal lobes may perform well on a Standardized Mini-Mental State Examination (SMMSE) because the screening tool is sensitive and specific to cognitive symptoms associated with Alzheimer’s disease.
By taking a global approach to self-monitoring, the app helps target the most appropriate tools for formal screening and assessment.
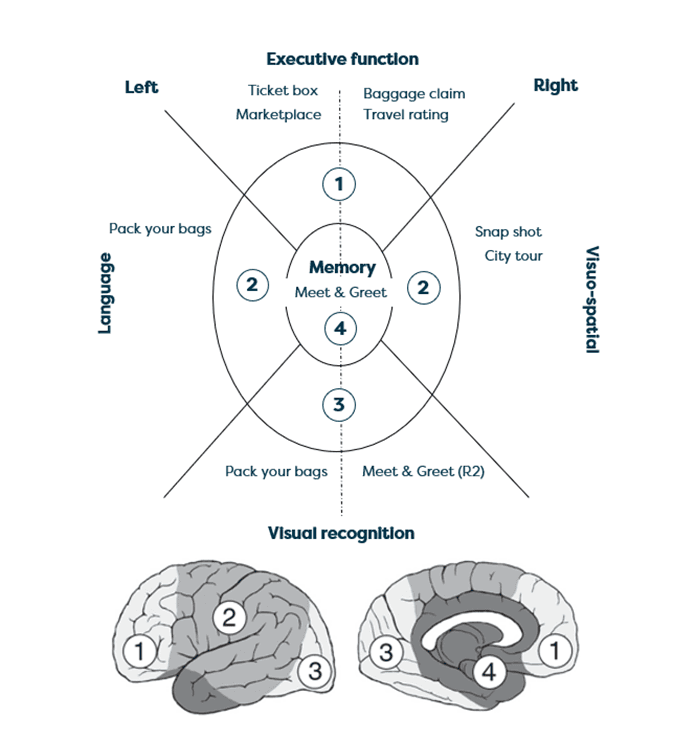
Cognitive domains targeted by each game
How do you interpret the results?
Scoring is based on the percentage of correct answers you give during each game. Results can be monitored over several months to inform progress over time. If the graph shows a downward trendline, it can validate symptoms you may have noticed.
Remember, the app is not a diagnostic tool. There are several reasons why results may be lower than expected. You can download a summary of the results and share these with your GP to start a conversation about the next steps.
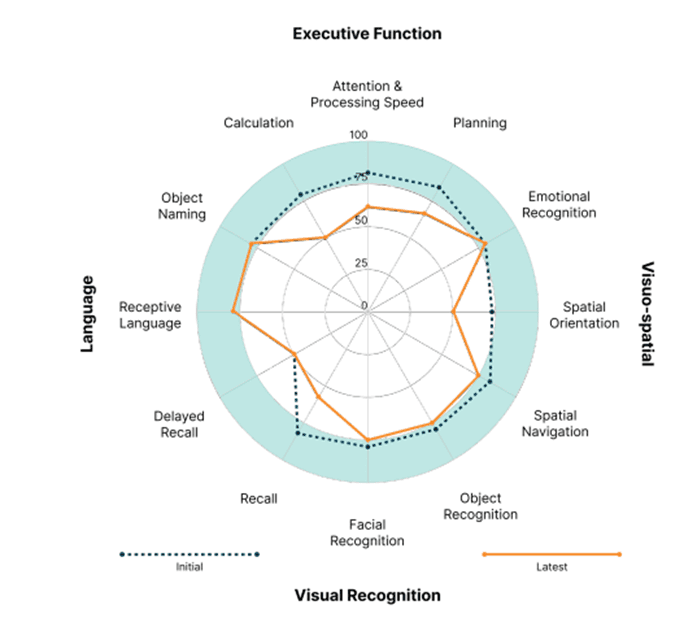
It is expected a person without cognitive impairment will show results between 75 and 100 per cent, allowing for random error.
If three or more cognitive processes score lower than 75%, consider formal cognitive screening.
As with validated cognitive testing, a person’s background, education level and visual or hearing impairment can impact their performance outcomes. These factors should be considered when reviewing results.
About the games
Baggage Claim
The user is presented with a bag with a specific colour, size and shape. They are asked to tap on this bag as it travels across the screen. There are three rounds: slow, medium and fast.
Cognitive process:
Attention: Users need to sustain attention to identify the correct target amongst competing stimuli. Variation in the frequency of the targets is used to manipulate difficulty.
Vigilance: Users must remain focused on all possible targets. Missed and incorrect targets are accounted for in the results.
Cognitive flexibility: As the rules change, users need to shift their thinking to identify new targets in each round.
Processing speed: Each round, the user must adapt to a variation in target speed.
Impulsivity: As difficulty increases, users need to override the desire to tap too quickly. This is measured by the number of incorrect taps and random anticipatory results.
Potential symptoms:
The person may:
- be easily distracted
- be unable to focus for long periods
- no longer be interested in activities that require sustained attention
- have difficulty with driving or operating machinery.
Related validated tests
Standardised Mini-Mental State Examination
- Attention - serial sevens
Montreal Cognitive Assessment (MoCA)
- Trail making test
- Attention
Frontal Battery Assessment (FAB)
Meet and Greet
The user is introduced to four travel companions in a tour group. They are provided with an image, a name and one fact about the person.
There are two rounds:
Round 1: Immediate recall The user is asked four multiple-choice questions about their tour companions.
Short break The user watches a mindfulness video to relax and clear their mind.
Round 2: Delayed recall The user is asked four multiple-choice questions about their tour companions.
Cognitive process:
Immediate recall: Users immediately recall new information.
Abstract thinking: Users answer non-direct questions.
Facial recognition: Users recognise the person’s face and match it with the correct information. Users are also asked to identify which person is not on the tour.
Delayed recall: Users repeat the same type of question after a two-minute delay.
Potential symptoms:
The person may have difficulty:
- remembering things, such as appointments, taking medications, information
- recognising people
- understanding more complex information.
Related validated tests
Standardised Mini-Mental State Examination
- Memory
- Delayed recall
Montreal Cognitive Assessment (MoCA)
- Memory
- Abstraction
- Delayed recall
GPCOG
- Information
- Recall
Pack your bags
The user is presented with tasks that test their ability to recognise items, name items and listen to instructions.
Round 1: The user is presented with items to pack. The user must choose appropriate items based on the day’s activity.
Round 2: The user is shown an object and asked to type the correct name of the object.
Round 3: The user is asked to recognise and sort objects based on verbal instructions.
Cognitive process:
Object recognition and temporal orientation: Users recognise and choose appropriate clothing to suit the weather.
Object naming: Users correctly recognise and name items.
Language comprehension: Users listen to and comprehend a verbal instruction.
Potential symptoms:
The person may have difficulty:
- recognising common or familiar items
- correctly naming items
- finding the right words (they may use descriptions instead)
- understanding and following conversations.
Related validated tests
Standardised Mini-Mental State Examination
- Naming
- Instruction
Montreal Cognitive Assessment (MoCA)
- Naming
- Language
GPCOG
- Information
- Recall
Ticket Box
The user is given a seating plan with limited clues to the seating numbers.
The user is asked to:
- find their seat
- work out the pattern of seating numbers and letters.
Cognitive process:
Recognise patterns: Users identify the number and letter pattern.
Problem-solving: Users find a solution to the question.
Planning: Users connect letters and numbers.
Potential symptoms:
The person may have difficulty:
- working through complex problems
- sequencing tasks, such as following a recipe
- managing their medications
- driving.
Related validated tests
Frontal Battery Assessment (FAB)
Montreal Cognitive Assessment (MoCA)
- Clock drawing
- Trail making
GPCOG
- Clock drawing
Snap Shot
The user is presented with an image of several 3D buildings or landmarks.
Round 1: The user is asked to identify buildings from above.
Round 2: The user needs to rotate a group of buildings to the correct orientation.
Cognitive process:
Spatial orientation
- Users mentally rotate shapes.
- Users identify the orientation of shapes.
- Users manipulate spatial information.
Potential symptoms:
The person may have difficulty:
- identifying specific objects amongst others
- perceiving depth (they may bump into furniture or doors)
- judging distance
- handwriting
- balancing (they may fall often)
- driving.
Related validated tests
Standardised Mini-Mental State Examination
- Copy design
- Sentence writing
- Folding paper exercise
Montreal Cognitive Assessment (MoCA)
- Copy cube
- Clockface
GPCOG
- Clockface
Marketplace
The user is asked to tap the correct notes and coins to purchase items at the market.
This game challenges the user to:
- calculate currency
- identify the correct notes and coins
- think flexibly as the notes and coins change with each country.
Cognitive process:
Calculation: Users demonstrate skills in addition and subtraction.
Possible symptoms
The person may have difficulty:
- paying bills
- banking
- paying for shopping
- managing finances and making complex financial decisions
- avoiding financial abuse.
Related validated tests
Standardised Mini-Mental State Examination
- Calculation - serial sevens
Montreal Cognitive Assessment (MoCA)
- Calculation— serial sevens
City Tour
The user is asked to find their way to and from a landmark navigating each intersection at a time.
This game challenges the user to:
- navigate the map using visual cues
- follow and understand the map
- navigate left or right turns
- mentally rotate the map to find their way back.
Cognitive process:
Spatial navigation: Users demonstrate wayfinding skills.
Possible symptoms
The person may have difficulty finding their way:
- in large shopping centres
- navigating when out walking
- when driving.
Related validated tests
Maze Navigation Test (MNT)
Travel Rating
The user is asked to look at images of people’s faces and correctly identify the expressed emotion.
This game challenges the user to identify other people’s emotions.
Round 1: Users are shown image of a whole face.
Round 2: Users are shown image of the eyes only.
Related cognitive domains
Emotion recognition: Users are asked to recognise emotion using visual cues.
Possible symptoms
The person may have difficulty:
- reading the emotional cues of others
- showing empathy.
Related validated tests
Frontal Battery Assessment (FAB)
Cognitive assessment for diverse population
Dementia Outcomes Measurement Suite
For people with English as a second language
Rowland Universal Dementia Assessment Scale (RUDAS)
For Aboriginal and Torres Strait Islander people
Kimberley Indigenous Cognitive Assessment tool (KICA)
Information for health professionals
Supporting risk reduction
Dementia is a complex syndrome describing several underlying conditions that impair a person's cognitive function across several cognitive domains 1. As one of the biggest contributors to disability worldwide, 1 dementia is a highly prevalent chronic condition and a major global health challenge. 2
In 2017, a global action plan was developed to take positive actions to reduce the significant impact of dementia. 1 One of these actions is a focus on risk reduction.
A significant amount of research from the last decade shows the potential for to reduce the risk of developing dementia or delay the onset of symptoms.3
Although we cannot definitively prevent dementia, there are many factors we can identify and manage to reduce our risk. These factors are known as modifiable risk factors and contribute to between 35 and 50 per cent of all dementia cases worldwide.3,4 By targeting modifiable risk factors through education and strategies, we can reduce the risk of developing dementia and keep people healthy and independent for as long as possible.5
What are these modifiable risk factors
A combination of medical and modifiable risk factors significantly influences our risk of developing dementia. Many of these factors are things we can identify, target and manage to reduce risk.
We now know that changes in the brain may begin up to 20 years before the first noticeable signs of dementia. Some factors appear more important at different stages of life. This suggests we should think about brain health throughout all stages of life, not only in old age. This is what we call a life-stage approach to dementia risk reduction.
Check-in quiz
GPs play a significant role in primary health prevention and promoting a life-stage approach to brain health. The Check-In Quiz helps identify the user’s modifiable risk factors.
The quiz asks the user a series of questions associated with modifiable risk factors. The user is presented with feedback on ‘Things to keep up’ and ‘Things you can try’. The user is encouraged to explore tips and strategies to optimise their brain health and set brain-healthy goals.
GPs can support their patients by:
- screening for and managing related health conditions
- providing access to health information and health promotion programs
- providing referrals to other health professionals to achieve their brain-healthy goals.
Responding to cognitive concern
This app is designed to support brain health conversations between GPs and their patients. These can be difficult conversations, especially when cognitive change might mean a diagnosis of dementia. However, when a person is ready to explore their cognitive concerns, they are more likely to approach family, friends and their GP first.6,10,18
GPs are well placed to recognise cognitive changes in their patients, as they have often developed a longer-term therapeutic relationship. Despite this, there are still low detection rates in primary care. 7
Many patients will receive a dementia diagnosis well after symptoms appear,1 with a quarter of Australian patients receiving a diagnosis in the moderate stage of the disease.8 Recent statistics show up to 58.7 per cent of people globally remain underdiagnosed or unaware of their diagnosis.9 Alzheimer’s Disease International reports up to 75 per cent of people lack a formal diagnosis, with significantly higher numbers in underdeveloped countries.9
Cognitive concerns should be taken seriously. It provides an ideal opportunity to start a conversation about brain health. Unpacking these concerns can be done in a staged approach over several scheduled appointments.
Benefits of early detection of cognitive change
Although there is no current cure for dementia, a formal diagnosis in its earliest stages is beneficial to the person and their care partners.10,11,12
When diagnosed in the early stages of dementia, the person can:
- understand the nature of their diagnosis
- access pharmacological treatment to delay symptoms
- adjust to the diagnosis through education and counselling
- access cognitive rehabilitation and timely support services
- determine future planning and decision-making 13, 14,15
- modify risk factors that contribute to disease progression 11
- make life changes to potentially slow the progression of symptoms
- delay admission to high-level care 11, 16
- Early diagnosis can also help reduce the stress and care burden on family members. 17
What is timely diagnosis
Timely diagnosis of dementia is a person-centred approach to diagnosis. The rights of the person and their unique circumstances are central to the diagnosis.18
A GP should allow time across several appointments:
- explore symptoms with the patient and their family
- undertake an appropriate, targeted assessment
- disclose a diagnosis at a time appropriate for that person.19
What to say to patients
Responding to concerns about symptoms (It is important not to brush off or dismiss concerns)
- Thank you for letting me know
- That must be worrying for you
- I can see this is worrying you
Finding out more information about changes
- Tell me more
- How long have you noticed the changes?
- How are these changes affecting you?
- Have other people also noticed these changes?
Ruling out acute illness (Delirium screen)
- Let's run a few tests to see if there is anything that can explain these changes
Responding to concerns about dementia
- There are a number of reasons you might be experiencing these symptoms
- We can take our time to explore, but first, let’s rule out any other causes
Scheduling more appointments (Take your time to unpack this at the right pace for the patient. Book another longer appointment)
- Let’s take our time to explore this a bit more over the next few weeks
- I will also book you in with our nurse to explore your concerns and take a baseline weight and urine test
Asking about risk
- Have you had any accidents or near misses when driving?
- Have you found yourself a bit lost when out of the house?
- Have you burnt any meals from leaving them on the stove?
- Have you lost your keys or locked yourself out of the house?
Checking for psychiatric symptoms
- Do you hear voices of people that you are unable to see?
- Are you worried about anyone trying to harm or take advantage of you?
- Are there strange things happening that you can’t explain?
Checking mood
- How would you describe your mood?
- How would you rate your mood out of 10?
- Would you describe your mood as low? How long have you been feeling like this?
- Do you feel safe?
- Do you have thoughts of harming yourself in any way? If yes, escalate for urgent referral to a local mental health service.
Assessing family support
- Would it be okay if I spoke to your family about your concerns?
- Is there someone you can bring to the next appointment?
- Is it okay if I talk to your family member while you are with the nurse?
Disclosing diagnosis
- The good news is the blood tests were normal and there are no tumours. However, we did find some brain changes that may explain the symptoms you are experiencing. And these changes look like a type of dementia.
- The tests confirm you have the early stages of dementia. (Show the cognitive test results, for example, clockface.)
Next steps
The Dementia Pathways Tool provides an intuitive yet comprehensive source of dementia-related information, tools, service directories and resources. It is publicly available and includes location-specific information on family and carer support, financial and legal issues, driving capabilities and powers of attorney.
BrainTrack was the winner of the 2023 ACT iAward in the Community/Not-For-Profit category, awarded jointly to Dementia Australia and Deakin University’s Applied Artificial Intelligence Institute.
About Dementia Australia
Dementia Australia (DA) is the peak body representing people living with dementia and their family carers. They provide information, counselling and support through the diagnostic pathway, from pre-diagnosis to the end stages of the disease. In line with global population health recommendations,1 a key strategy for Dementia Australia is to support access to a timely diagnosis of dementia.20
Dementia Australia is well-known for developing innovative technology to both aid in the understanding of dementia and improve the support experience of people living with dementia and their families. These technologies include the use of gamification, virtual reality, avatars and novel digital applications. This innovation is underpinned by research and evidence, and products are rigorously evaluated through independent university evaluations.
This project is funded by the Department of Health under the National Dementia Support Program.
References
- World Health Organization. Global action plan on the public health response to dementia 2017–2025. 2017 (pp. Licence: CC BY-NC-SA 3.0 IGO). Geneva.
- Alzheimer’s Disease International. World Alzheimer Report 2015. The Global Impact of Dementia An analysis of prevalence, incidence, cost and trends. 2015.
- Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention and care. Lancet. 2017.;390(10113):2673-734
- Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurol. 2013;13(8):788-94.
- Langa KM, Larson EB, Crimmins EM, Faul JD, Levine DA, Kabeto MU, Weir DR. A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Intern Med. 2017;177(1):51-8.
- Hamilton-West, K., Milne, A., Chenery, A., & Tilbrook, C. Help-seeking in relation to signs of dementia: A pilot study to evaluate the utility of the common-sense model of illness representations. Psychology, Health & Medicine, 2010;15(5), 540-549.
- Lang, L., Clifford, A., Wei, L., Zhang, D., Leung, D., & Augustine, G. et al. Prevalence and determinants of undetected dementia in the community: a systematic literature review and a meta-analysis. BMJ Open, 2017;(2), e011146. doi: 10.1136/bmjopen-2016-011146
- Black, C., Woodward, M., Ambegaonkar, B., Philips, A., Pike, J., & Jones, E. et al. Quantifying the diagnostic pathway for patients with cognitive impairment: real-world data from Australia. International Psychogeriatrics,2019;32(5), 601-610. doi: 10.1017/s1041610219001856
- Gauthier, S., Rosa-Neto, P., Morais, J., & Webster, C. World Alzheimer Report 2021: Journey through the diagnosis of dementia. London, England: Alzheimer’s Disease International. 2021.
- Birt, L., Poland, F., Charlesworth, G., Leung, P., & Higgs, P. Relational experiences of people seeking help and assessment for subjective cognitive concern and memory loss. Aging & Mental Health, 2019;24(8), 1356-1364.
- Panegyres, P., Berry, R., & Burchell, J. Early dementia screening: Review. Diagnostics,2016; 6(6).
- Luck, T., Luppa, M., Sieber, J., Schomerus, G., Werner, P., König, H., & Riedel-Heller, S. Attitudes of the German General Population toward Early Diagnosis of Dementia – Results of a Representative Telephone Survey. Plos ONE, 2012;7(11), e50792. doi: 10.1371/journal.pone.0050792
- Robinson, L., Tang, E., & Taylor, J. Dementia: timely diagnosis and early intervention. BMJ,2015; 350(jun15 14), h3029-h3029.
- Alzheimer’s Disease International. The benefits of early diagnosis and intervention. Retrieved from http://www.alz.co.uk/research/world-report-2011. 2011.
- Dubois, B., Padovani, A., Scheltens, P., Rossi, A., & Dell’Agnello, G. Timely Diagnosis for Alzheimer’s Disease: A Literature Review on Benefits and Challenges. Journal Of Alzheimer's Disease, 2015;49(3), 617-631.
- Ng, N., & Ward, S. Diagnosis of dementia in Australia: a narrative review of services and models of care. Australian Health Review, 2019;43(4), 415.
- Helvik, A., Engedal, K., Šaltytė Benth, J., & Selbæk, G. Time from Symptom Debut to Dementia Assessment by the Specialist Healthcare Service in Norway. Dementia And Geriatric Cognitive Disorders Extra, 2018;8(1), 117-127.
- Brooker, D., Fontaine, J., Evans, S., Bray, J., & Saad, K. Public health guidance to facilitate timely diagnosis of dementia: ALzheimer's COoperative Valuation in Europe recommendations. International Journal of Geriatric Psychiatry, 2014;29(7), 682-693.
- Watson, R., Bryant, J., Sanson-Fisher, R., Mansfield, E., & Evans, T. What is a ‘timely’ diagnosis? Exploring the preferences of Australian health service consumers regarding when a diagnosis of dementia should be disclosed. BMC Health Services Research, 2018;18(1).
- Dementia Australia. A roadmap for quality dementia care; Parliamentary Friends of Dementia paper. 2021.
